A new analysis of over 2 million patient visits and encounters from 228 hospitals in 40 states by research firm Strata Decision Technology is the first to provide a detailed view of the level of reduction in patients accessing healthcare and the associated impact on the health of patients and the nation’s hospitals. The study reveals just how significant the wave of delayed care is that has built up during the COVID-19 pandemic – and how many of those patients may be unable to pay when they do seek care due to a loss of insurance coverage.
Strata analyzed 2 million patient visits and procedures from 51 healthcare delivery systems in 40 states, with varying rates of COVID-19 cases in their 228 hospitals. Analysts then compared patient encounters during a two-week period in March and April 2020 to the comparable period last year. The analysis reveals that across all service lines and in every region of the country there was an average decrease in the number of unique patients who sought care in a hospital setting of 54.5%. The sharp drop in encounters is linked to the cancelation of elective surgeries during this time period, along with resource constraints and ongoing concerns for the safety of patients and staff.
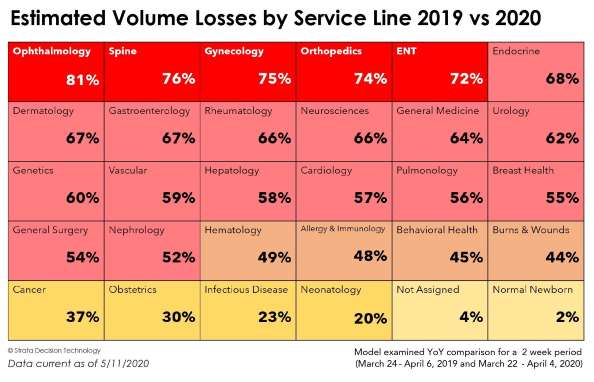
Millions of patients who put off care or had it delayed during the pandemic can soon be expected to flood hospitals and physician offices seeking care. Clinical service lines that saw the sharp drops in patient encounters included those with life-threatening illnesses such as a 57% decrease in cardiology, and a 55% decrease in breast health with a 37% decline in cancer care overall. Many facilities will likely be hard-pressed to handle the resulting surge in patients while simultaneously maintaining capacity for COVID-19 patients.
Major Declines in Top 10 Inpatient Procedures
Inpatient procedures and surgeries account for the majority of revenue for hospitals. The top 10 procedures account for over 50% of the total payments made to hospitals. In this category there were significant declines in the number of hip (-79%) and knee (-99%) replacement surgeries as well as in spinal fusions (-81%) and repair of fractures (-38%). Coronary stents (-44%) and diagnostic catherization (-65%) also saw significant declines. Overall diagnostic volume declined by 60%. Both normal delivery (1%) and C-section (2%) saw increases. Mechanical ventilation increased by 24% due to treatment of COVID-19 patients.
Reduction in the Number of People Accessing Care
Among the findings are significant recent reductions in patient encounters (both inpatient and outpatient) for so-called elective care that is crucial to maintaining the health of millions of Americans. Drops in patient volume are shown below for several of the 225 Clinical Care Family definitions determined using the Sg2 Care Grouper.
Access to clinical care for patients with life-threatening conditions declined significantly including congestive heart failure (-55%), heart attacks (-57%) and stroke (-56%). Access by patients for chronic conditions also fell for patients with hypertension (-37%) and diabetes (-67%). The high volume patient visits and procedures that dropped the most were for cataracts (-97%), sleep apnea (-91%) and osteoarthrosis (-88%) and glaucoma (-88%). Additionally, health screenings that are designed to provide early detection but are often seen as less urgent were down significantly in volume, increasing the risk of undiagnosed disease. Preventive wellness visits, gynecologic wellness and screenings, and GI benign neoplasms and polyps—which includes colonoscopies with removal of polyps—all saw volumes drop by over 75% in the cohort group.
“Hospitals across the country are eager to open their doors to elective procedures so they can serve their community, care for their patients, and survive economically but how they get there is literally a hundred-billion-dollar question,” said Dan Michelson, CEO of Strata Decision Technology. “Many facilities will likely be hard-pressed to handle the surge while simultaneously maintaining capacity for COVID-19 patients. Having visibility into patient volumes across all of their service lines is key to understanding how to safely engage patients while balancing the clinical, operational and financial complexity and pressures imposed by COVID-19. The data is clear, however, that the initial relief package given to hospitals and healthcare providers will not be enough. More funding will be needed to ensure that they can keep their doors open to provide essential care for the communities they serve while still preparing and caring for COVID 19 patients.”
Revenues Down by $60.1 Billion/Month; Uninsured Patients up by 114%
The massive drop in patient visits and procedures during the pandemic has led directly to unprecedented financial losses. Health systems in the study cohort lost an estimated $1.35 billion in revenue during the 2-week study period compared to the prior year. Extrapolating the drop in volume from the cohort to a national view would be the equivalent revenue loss of $60.1 billion per month for hospitals nationwide.
Adding to the crisis, the Strata study found that the number of uninsured or self-pay patients has increased dramatically in the last 90 days, mirroring the rise in the national unemployment rate. In January, 7% of all inpatient and outpatient encounters in the study cohort were with patients who lacked health insurance. By April that figure had risen to 11%, and early results from May indicate 15% of all patients in the cohort are now uninsured, an increase of 114% in just 90 days. Many of these can be expected to end up on Medicaid rolls, further straining state budgets.